Zamykanie naczynek marki: innowacyjne metody i kluczowe korzyści
Trends and Innovations in Vascular Closure Devices
I. Introduction
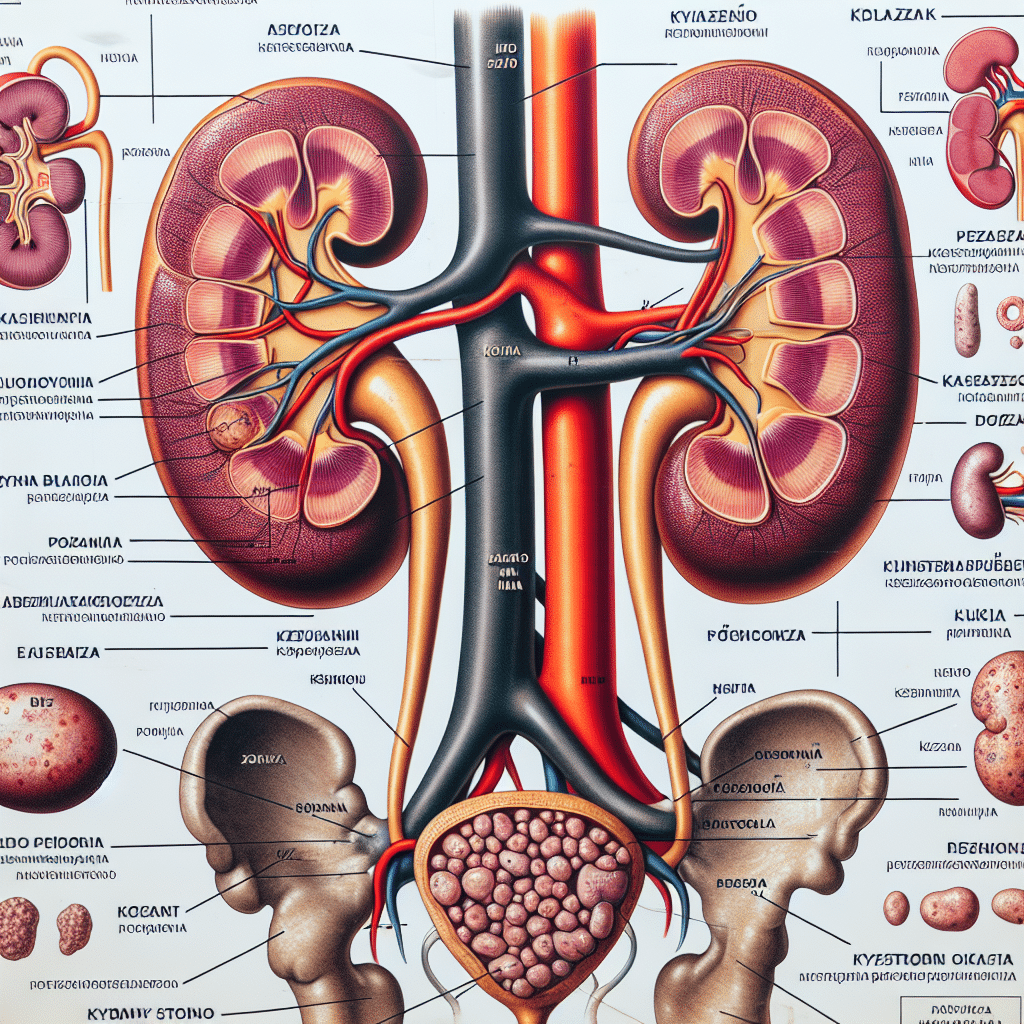
A. Overview of Vascular Closure Devices
Vascular closure devices are medical instruments designed to seal the puncture site in blood vessels after diagnostic and interventional procedures. They aim to improve patient outcomes by reducing complications associated with manual compression.
These devices come in various forms, such as sealants, sutures, plugs, and closure discs. They are used to achieve hemostasis efficiently and expedite the recovery process.
B. Importance of Effective Vascular Closure
Effective vascular closure is crucial for minimizing the risk of bleeding, hematoma formation, and access site complications. It ensures that the patient can safely resume normal activities and prevents the need for prolonged bed rest or hospitalization.
Uncontrolled bleeding or inadequate closure can lead to various complications, ranging from minor bruising to life-threatening events such as pseudoaneurysm formation or arterial thrombosis.
C. Need for Innovation in Vascular Closure Methods
While traditional methods like manual compression have been the standard for decades, there is a growing need for innovative solutions in vascular closure. The limitations, challenges, and associated risks of these traditional methods drive the demand for new technologies.
Innovation in vascular closure methods aims to improve patient comfort, reduce complications, enhance procedural efficiency, and provide healthcare practitioners with more reliable and effective options.
II. Traditional Methods of Vascular Closure
A. Manual Compression
Manual compression is the oldest and most widely used method of achieving hemostasis after arterial puncture. It involves applying pressure manually to the puncture site until bleeding ceases. However, it has several limitations and risks.
1. Procedure and Limitations
The procedure of manual compression involves applying firm pressure with the hand or a sandbag over the puncture site. The pressure is maintained for a duration determined by the operator’s discretion, typically ranging from 10 to 30 minutes.
However, manual compression is operator-dependent, and the effectiveness can vary based on the skills and experience of the healthcare provider. Additionally, prolonged compression times can lead to patient discomfort, delayed ambulation, and increased healthcare costs.
2. Challenges and Risks
Manual compression presents various challenges and risks. In cases where the artery is larger, calcified, or heavily diseased, achieving hemostasis through manual compression alone may be difficult or time-consuming.
Complications associated with manual compression include hematoma formation, retroperitoneal bleeding, vessel spasm, and nerve injury. The risk of re-bleeding or late closure failure is also higher compared to other closure methods.
B. Mechanical Compression Devices
Mechanical compression devices have been introduced as an alternative to manual compression. These devices apply pressure on the puncture site using external mechanisms, reducing the operator’s reliance on manual force.
1. Types and Mechanisms
There are various types of mechanical compression devices available, such as vascular compression pads, clotting sponges, and inflatable balloons. These devices exert pressure on the arterial site for a specific duration, ensuring hemostasis.
The mechanisms of these devices involve the application of either constant pressure or intermittent pressure, with some devices allowing customization of pressure settings based on patient-specific factors.
2. Efficacy and Limitations
Mechanical compression devices have shown improved efficacy compared to manual compression in achieving hemostasis. They provide consistent pressure, leading to faster closure times and reduced complications.
However, these devices are not suitable for all patients, particularly those with anatomical variations or significant vessel tortuosity. Additionally, the cost of these devices and the need for training in their proper use can limit their widespread adoption.
III. Emerging Techniques in Vascular Closure
A. Percutaneous Closure Systems
Percutaneous closure systems represent a significant advancement in vascular closure technology. They involve the use of devices specifically designed to seal the puncture site through percutaneous means, without sutures or manual compression.
1. Development and Advantages
Percutaneous closure systems have evolved from simple plugs and sutures to more sophisticated devices utilizing various mechanisms, such as collagen-based sealants, bioabsorbable anchors, and shape memory alloy clips.
These systems provide several advantages, including shorter closure times, reduced complications, improved patient comfort, and decreased healthcare costs. They offer a more reliable and predictable method of achieving hemostasis.
2. Different Types and Applications
There are different types of percutaneous closure systems available, each catering to specific procedural needs and vessel sizes. Some systems are suitable for small-diameter vessels, while others are designed for larger arterial access sites.
These systems find applications in various interventional procedures, including cardiac catheterization, peripheral vascular interventions, and neurovascular interventions.
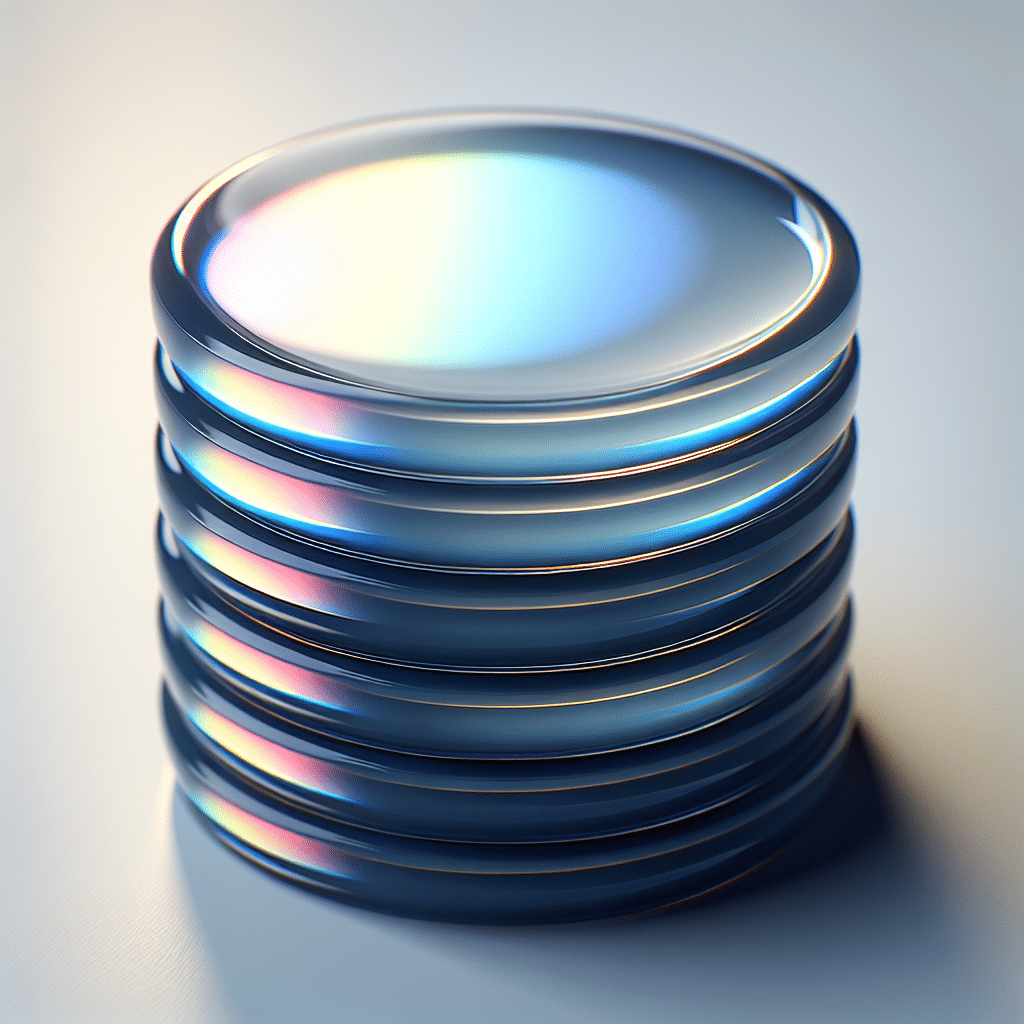
B. Nitinol-based Closure Devices
Nitinol-based closure devices are another innovative solution in vascular closure. Nitinol, a nickel-titanium alloy, possesses unique properties that make it suitable for use in closure devices.
1. Working Principle and Benefits
Nitinol-based closure devices work on the principle of shape memory and superelasticity. These devices can be compressed and inserted through a small puncture site, expanding and exerting pressure when deployed at the arterial access site.
The benefits of Nitinol-based closure devices include ease of use, reduced compression times, enhanced patient comfort, and reliable hemostasis. The unique properties of Nitinol allow for optimal vessel wall apposition and reduce the risk of complications.
2. Effectiveness and Clinical Applications
Studies have demonstrated the effectiveness of Nitinol-based closure devices in achieving rapid hemostasis and reducing complications compared to manual compression. These devices have found applications in various endovascular procedures, such as angiography, angioplasty, and stenting.
C. Bioresorbable Vascular Scaffolds
Bioresorbable vascular scaffolds (BVS) are a novel approach to vascular closure. These devices are designed to provide temporary support to the arterial access site while promoting hemostasis and subsequent healing.
1. Role in Vascular Closure
BVS are made of bioresorbable materials that gradually degrade over time, allowing the artery to regain its normal function. They act as a physical barrier, preventing bleeding and maintaining vessel patency until the puncture site heals.
Once the healing process is complete, the scaffold is completely absorbed by the body, eliminating the need for its removal and reducing the risk of long-term complications.
2. Advancements and Future Prospects
Ongoing research and development in bioresorbable vascular scaffolds aim to improve their mechanical properties, biocompatibility, and ease of use. Advancements in materials science and engineering have led to the development of next-generation BVS with enhanced performance and greater clinical acceptance.
IV. Benefits of Innovative Vascular Closure Methods
A. Reduced Complications and Risks
Comparing traditional methods with innovative vascular closure techniques reveals significant reductions in complications and risks.
1. Comparing Traditional vs. Innovative Methods
Studies have demonstrated lower rates of access site complications, such as hematoma formation, infection, and local vascular complications, when using innovative closure methods compared to manual compression.
The use of percutaneous closure systems, Nitinol-based devices, and BVS has shown superior outcomes and a lower incidence of adverse events.
2. Clinical Studies and Evidence
Clinical studies have supported the effectiveness of innovative closure methods in reducing complications and improving patient outcomes. These studies provide evidence of the benefits associated with the adoption of these new technologies.
B. Enhanced Patient Comfort and Satisfaction
Innovative vascular closure methods prioritize patient comfort and satisfaction by minimizing pain and discomfort associated with the closure process.
1. Minimizing Pain and Discomfort
Compared to traditional methods, which often involve prolonged compression times, innovative techniques significantly reduce patient discomfort. Percutaneous closure systems, Nitinol-based devices, and BVS offer faster hemostasis and enable patients to ambulate sooner.
2. Patient Feedback and Case Studies
Patient feedback and case studies support the claim that innovative vascular closure methods enhance patient satisfaction. Patients report less pain, reduced anxiety, and easier post-procedure recovery compared to traditional closure methods.
C. Improved Procedural Efficiency and Workflow
Innovative vascular closure methods contribute to improved procedural efficiency and workflow in healthcare settings.
1. Faster Hemostasis and Ambulation
Percutaneous closure systems, Nitinol-based devices, and BVS enable faster hemostasis, allowing patients to ambulate sooner. This reduces the duration of hospital stays and enables healthcare providers to treat more patients within a given timeframe.
2. Economical Advantages for Healthcare Providers
Innovative closure methods can offer economical advantages to healthcare providers by reducing resource utilization, such as bed occupancy and staff time. The decreased incidence of complications also translates to cost savings by avoiding additional interventions or extended hospital stays.
V. Key Considerations for Implementing Innovative Vascular Closure
A. Learning Curve and Training Requirements
Implementing innovative vascular closure methods requires adequate training and skills development among healthcare providers.
1. Skills and Expertise Needed
Healthcare providers must acquire the necessary skills and expertise to perform these procedures safely and effectively. Training programs can provide hands-on experience and guidance on device selection, deployment techniques, and troubleshooting.
2. Training Programs and Continued Education
Training programs and continued education opportunities ensure that healthcare providers stay updated with the latest advancements in vascular closure devices and techniques. Regular skill assessments and competency evaluations further enhance patient safety and procedural outcomes.
B. Cost Analysis and Reimbursement
The implementation of innovative vascular closure methods may require a thorough cost analysis and consideration of reimbursement policies.
1. Initial Investment vs. Long-term Benefits
While the initial investment in these devices may be higher than traditional methods, the long-term benefits, such as reduced complications, shorter hospital stays, and improved patient outcomes, can outweigh the costs.
2. Insurance Coverage and Reimbursement Policies
Understanding insurance coverage and reimbursement policies is crucial for the successful implementation of innovative closure methods. Collaborating with insurance providers and staying up-to-date with policy changes ensure appropriate reimbursement for these procedures.
C. Regulatory Challenges and Approval Process
Introducing innovative vascular closure methods into clinical practice requires navigating regulatory challenges and securing appropriate approvals.
1. Approval Criteria and Clinical Trials
The approval process for these devices involves demonstrating safety, efficacy, and clinical benefits through rigorous testing and clinical trials. Meeting regulatory approval criteria is essential to ensure patient safety and device effectiveness.
2. Regulatory Authorities and Guidelines
Familiarizing healthcare providers with the regulatory authorities and guidelines governing vascular closure devices is essential. Compliance with regulatory requirements ensures that these devices meet established safety and performance standards.
VI. Case Studies and Success Stories
A. Real-life Examples of Successful Vascular Closure Procedures
Real-life case studies provide valuable insights into the successful implementation of innovative vascular closure methods. These examples highlight the benefits, challenges, and outcomes associated with these procedures.
B. Testimonials from Patients and Healthcare Practitioners
Testimonials from patients and healthcare practitioners offer firsthand accounts of their experiences with innovative vascular closure methods. These narratives provide perspective on the impact of these techniques on patient care and procedural outcomes.
VII. Future Prospects and Innovations in Vascular Closure
A. Ongoing Research and Development
Ongoing research and development efforts focus on further improving vascular closure techniques and devices. Collaborative efforts between clinicians, engineers, and researchers aim to address limitations and introduce more advanced solutions.
B. Potential Breakthrough Technologies
Researchers are exploring potential breakthrough technologies in vascular closure, such as bioactive sealants, robotic-assisted closure devices, and targeted closure methods. These innovations hold promise for further enhancing patient outcomes and procedural efficiency.
C. Anticipated Impact on Clinical Practice
The adoption of innovative vascular closure methods is expected to have a significant impact on clinical practice. These techniques offer safer, more efficient, and patient-centered alternatives to traditional closure methods, transforming the standard of care in vascular interventions.
VIII. Conclusion
A. Summary of Key Findings
The field of vascular closure devices continues to evolve, with innovations aimed at improving patient outcomes and procedural efficiency. Percutaneous closure systems, Nitinol-based devices, and bioresorbable scaffolds offer promising solutions in achieving rapid and reliable closure.
B. Importance of Continual Advancement in Vascular Closure Techniques
Continual advancement in vascular closure techniques is essential for staying at the forefront of patient care. Novel technologies reduce complications, enhance patient comfort, and optimize procedural efficiency, leading to better clinical outcomes.
C. Final Thoughts on the Future of Vascular Closure
The future of vascular closure is exciting, with ongoing research, development, and innovation. Emerging technologies and breakthroughs hold the potential to revolutionize clinical practice and set new standards for vascular closure.
Artykuł dotyczy innowacyjnych metod zamykania naczynek marki, które mogą przynieść kluczowe korzyści dla Twojej skóry. Zachęcam do kliknięcia w poniższy link, aby dowiedzieć się więcej na temat tych nowatorskich rozwiązań: [link]: https://callofbeautydayspa.pl/zabiegi/laserowe-zamykanie-naczynek-glowica-dye-vl/.